Being a patient in a mental health hospital: Debunking the myths
The following story is from a recent patient, describing her struggles, experience and journey.
DISCLAIMER: talks of suicide
As I found myself on my hands and knees on the floor of my shower, naked, wet and dry retching into an abyss, I knew I couldn't go to work that day.
Years of faking 'being okay' and 'looking normal' had come to an end. This moment was the tail end of years of trying to cope with crippling anxiety, depression and emotional flashbacks. It was the moment my body and mind just said 'We can't do this anymore. You have to stop. We are broken'. That was February 2018.
Until this point, I'd held my highly functional self together with all sorts of coping mechanisms; counselling, meditation, naturopathy, self medicating with pain medication (for physical issues), alcohol, exercise, denial, compartmentalisation and 'keeping busy' (a favourite of many high functioning people). They all worked to varying degrees, for a time, before the anxiety, panic and misery would just come back with more force and it got harder and harder to keep it under control.
I don't like to say that I broke. I prefer to describe that I hit a wall and didn't have the resources to climb, dig underneath or break through. So, after much heartache and swallowing bitter pills, I sent myself off to a psychiatrist and asked (actually it was more like begged) for help.
I was diagnosed initially with panic disorder and OCD. [Sidenote: most people are misdiagnosed initially...it's pretty normal. My {extremely awesome} psychologist later recognised the signs of Complex Post Traumatic Stress Disorder]. At my request, I was prescribed with an anti-depressant (Fluoxetine), because there was nothing else left to try or lose. The meds were incredibly helpful and totally worth the short term side effects.
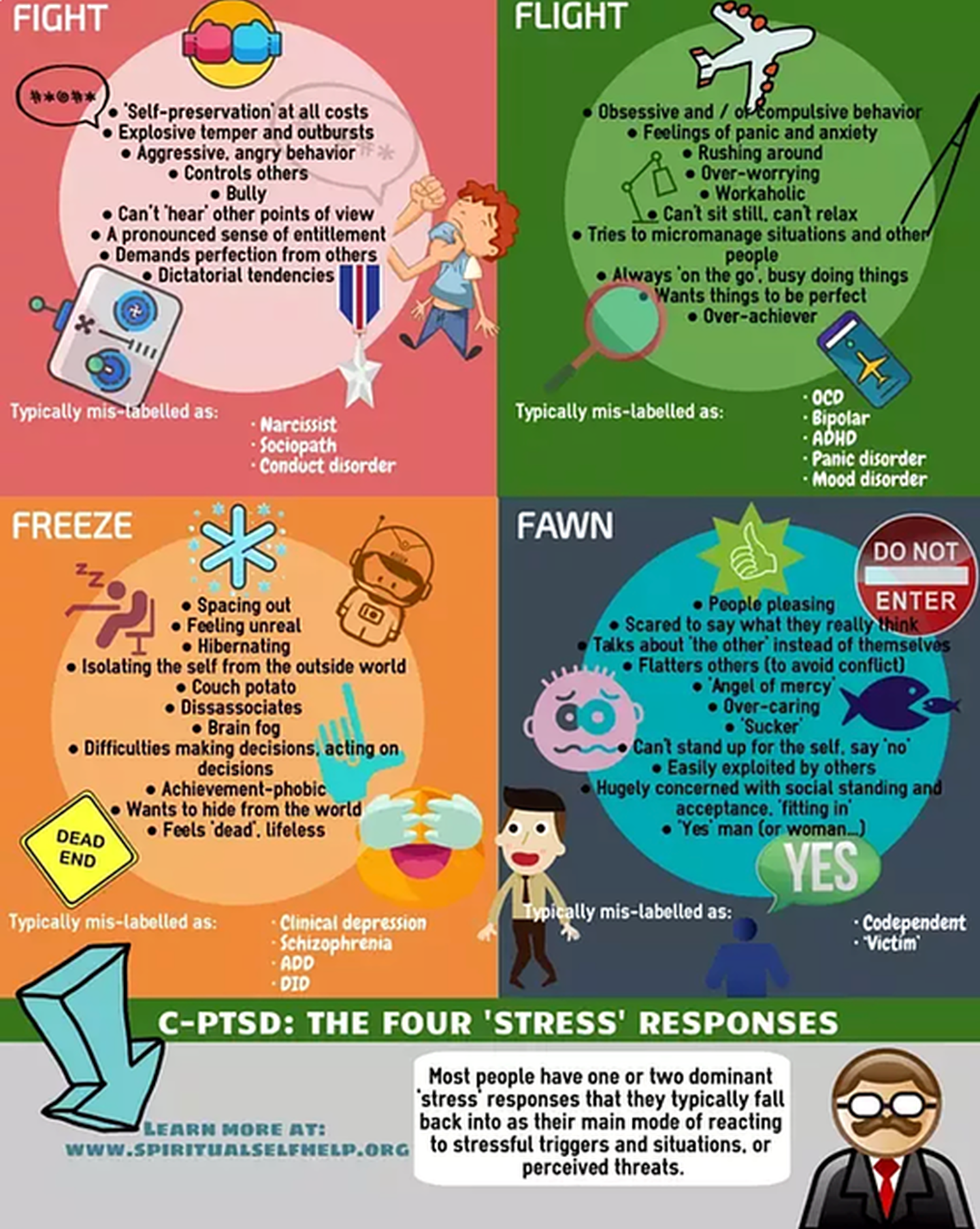
I accidentally came across this infographic about C-PTSD, which was a massively helpful light bulb moment. I tended to fit into the Flight/Freeze and Fawn categories:
All the time, I was honestly shitting myself:
'How the fuck did I get here?'
'How is this happening to me?'
'How can I end this pain?'
'Will this ever end?'
These were questions I asked myself every day. I knew I needed help, but the thought of going to hospital was terrifying. There was literally no formal information about it available, and all I could get was second hand snippets from (military) friends. Worse still, I had images in my mind of catatonic, dribbling patients, or people muttering to themselves while staring blankly at a wall, or even worse, strapped to a bed in isolation and sedated; visual projections of how mental health hospitals are presented in movies.
Then I caught a break. I discovered I had a friend who was getting in-patient treatment for severe PTSD. I called him and asked him all the questions I could, and once I was better informed, I felt safe enough to ask to be admitted into a mental health hospital.
{Disclaimer: This is about my experience. Others may have different experiences in mental health hospitals}
When my husband drove me to the hospital (South Coast Private in Wollongong), I was still shitting myself. Hitting rock bottom is extremely frightening, isolating, terrifying and feels hopeless and lonely. We arrived, checked in, my husband and I said our goodbyes for the next four weeks, then I was taken to my room (thankfully private) and taken through the in-processing procedure.
I was required to fill in a bunch of forms in my own time (my brain wasn't functioning, and basic form filling took on a totally new version of hard), hand in all sharps and cords (it's amazing how many cords one has these days; phone charger cables, laptop cables, hairdryers, robe ties). I joked with the nurse that the last method I would choose to kill myself would be hanging...driving my car into a tree was the usual thought. We had a laugh about that, and it was nice to talk openly about my thoughts for a change.
The plan was that I would take part in the three week small group PTSD course, which started about four days after my arrival. I spent the first 48 hours sleeping and eating. That was it. I was so utterly exhausted, and having all responsibilities removed from me was just what I needed. I was checked on by a nurse every two hours, I went to the dining room to eat three times a day and chose a table for one (the hospital was SOOOOO good at letting you be alone in a room full of people) as I didn't want to talk to anyone. I'd wear my headphones and read my book to make extra sure everyone got the message to leave me alone.
Once I was allocated to a group for the PTSD course, and actually met a few people, I felt safer to venture out of my room into the public spaces. The floor (not ward) I was on had two wings (with only 18 rooms I think) and in between, a central public relaxing space, next to the nurses desk. There was a pharmacy dispensary and a small area for a coffee machine and snacks. There were plenty of books, DVDs, a big TV, lots of meditative colouring in material. Everywhere had CCTV cameras (except your room), so the staff could see where everyone was at all times.
My floor was restricted to only emergency responders, nurses and military, which made it feel safe (for me), being around like minded people with similar backgrounds. I described it as feeling like the Officers Mess, but instead of stewards, we had nurses and instead of the bar, we had the pharmacy.
The rest of the hospital (which was a converted hotel) had a dining room, an art room, a gym, a large outdoor relaxing area with sun lounges and comfy chairs, a laundry (for you to wash your own clothes) and a bunch of rooms where group classes were carried out. Day leave was restricted at first, but after four days, I could sign out and go for walks to the beach, or go to cafes etc. On my second, longer stay, I took my bike and went for long bike rides.
A typical day when attending group classes (four days of the week) went like this:
- Up at 7.30am
- Meds
- Breakfast
- Group class for 90-120 mins
- Lunch
- Group class again
- Own time to meet with psychiatrist/psychologist, do homework, chill, sleep, exercise, do art etc
- Dinner
- Chill
- Meds
- Bed
The other days were spent doing larger informative group classes on wellness, yoga classes, gym classes and relaxing/sleeping/own time stuff.
As the four weeks progressed, my inner 'high alert' system started to calm down, my meds were adjusted to include night time sedatives to help me sleep properly, relaxants to help stop me clenching my jaw at night during nightmares, and I started to get educated on what was happening to me. I learned so much.
The shame and embarrassment I had initially felt disappeared as I learned that my illness was no different to someone with a broken leg, or with another treatable disease. I began to talk to others who had very similar experiences and realised that it wasn't just me. I was helped to feel safe(er) in my own skin and learned that all the symptoms I had been experience had a cause and a treatment. I was treated with utter respect, dignity, kindness and compassion. I felt safe at all times (as nobody could access my room except for staff). The staff were nothing short of incredible. I gained a completely new level of respect for mental health nurses.
By the time I left, I had a new found self respect and some degree of certainty on a way forward. I knew it was going to be a hard journey, but I felt confident that I had the right support team to help me. I learned the most important thing: I was not, had never been, and will never be alone in this.
I still wasn't well, and was scheduled to return at a later date to complete eight weeks of one-on-one intensive therapy. So I clung on to that hope. That I would come back and be helped, guided and reassured by these amazing professionals (and people I had connected with during our times of vulnerability) and heal my wounded mind and soul. But that's a story for another day.
love, S xxx
If you are experiencing familiar emotions and seeking help, do not hesitate to reach out.
CALL 1800 250 000 to find out how we can help.